If we have an allergy to peanuts, strawberries or dairy, we are quick to blame our immune systems. But when we enjoy a diverse diet without any adverse reaction, we generally don’t realize that this is also the immune system’s doing. Our blissful freedom from treating steak or cabbage – essentially foreign material – as a hostile invader is due to the immune mechanism known as oral tolerance. Though this tolerance is vital for our survival, its precise machinery had remained elusive, despite years of research. Now, a Nature study from Dr. Ranit Kedmi’s team at the Weizmann Institute of Science has resolved a long-standing paradox surrounding oral tolerance and revealed the cellular network that is responsible. These findings may help researchers understand this network’s malfunctions, which underlie food allergies and sensitivities and disorders such as celiac disease.
Tolerance to food begins to develop in the womb, as the fetus’s immune system is being exposed to substances derived from food consumed by the mother. It continues to mature during nursing and as the child begins to eat solid food, as well as through interactions with beneficial gut bacteria, which produce their own potential allergens that the immune system must learn to ignore.
For years, tolerance to food was thought to be orchestrated by immune cells called dendritic cells. These cells, which earned their discoverer, Ralph Steinman, the 2011 Nobel Prize, are major directors of the immune system’s attacks. In infection, these cells chop up microbes and present their bits and pieces to other cells, triggering an assault by the immune system. But the prevailing view of oral tolerance held that, after checking out digested food, they could instead decide to keep that assault at bay, instructing the immune cells to stand down and suppress any action. Strangely, however, when researchers eliminated the suspected subset of dendritic cells in animal models, oral tolerance still developed.
""If an aggressor fires across the border, he will be swiftly neutralized, peace accords notwithstanding. The immune system operates on a similar principle"
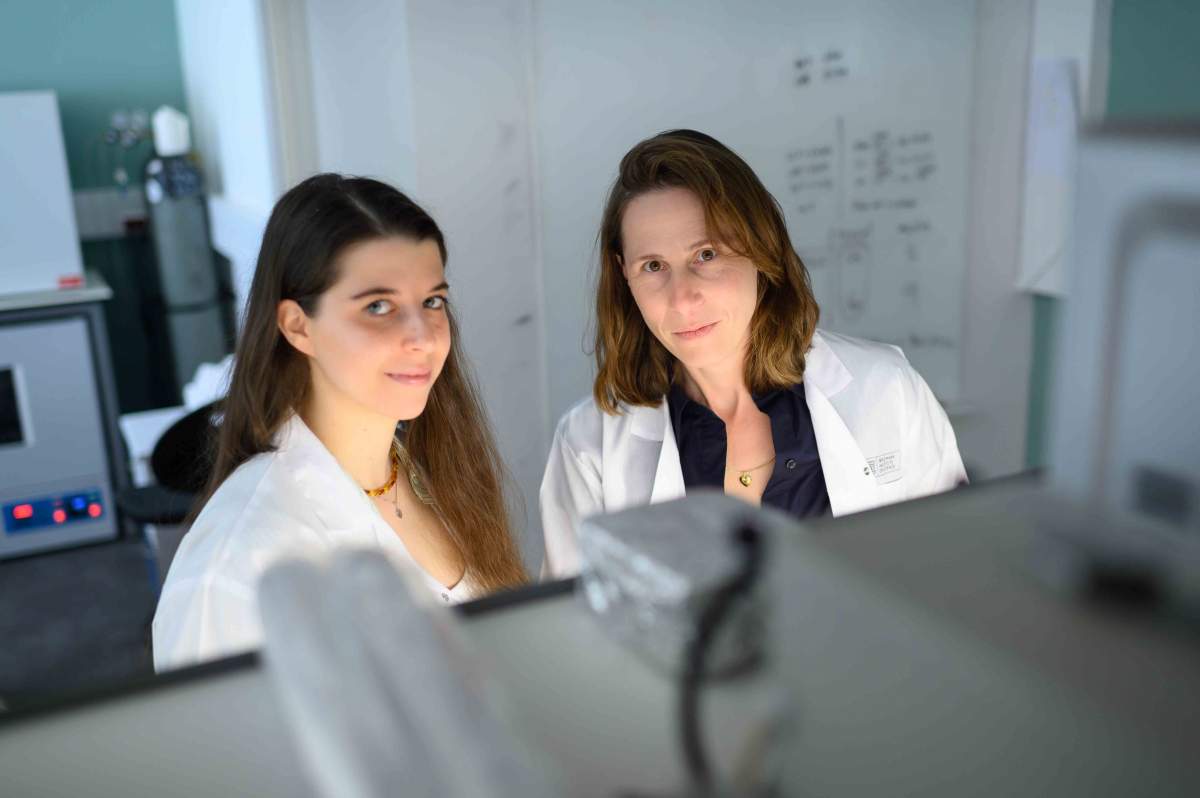
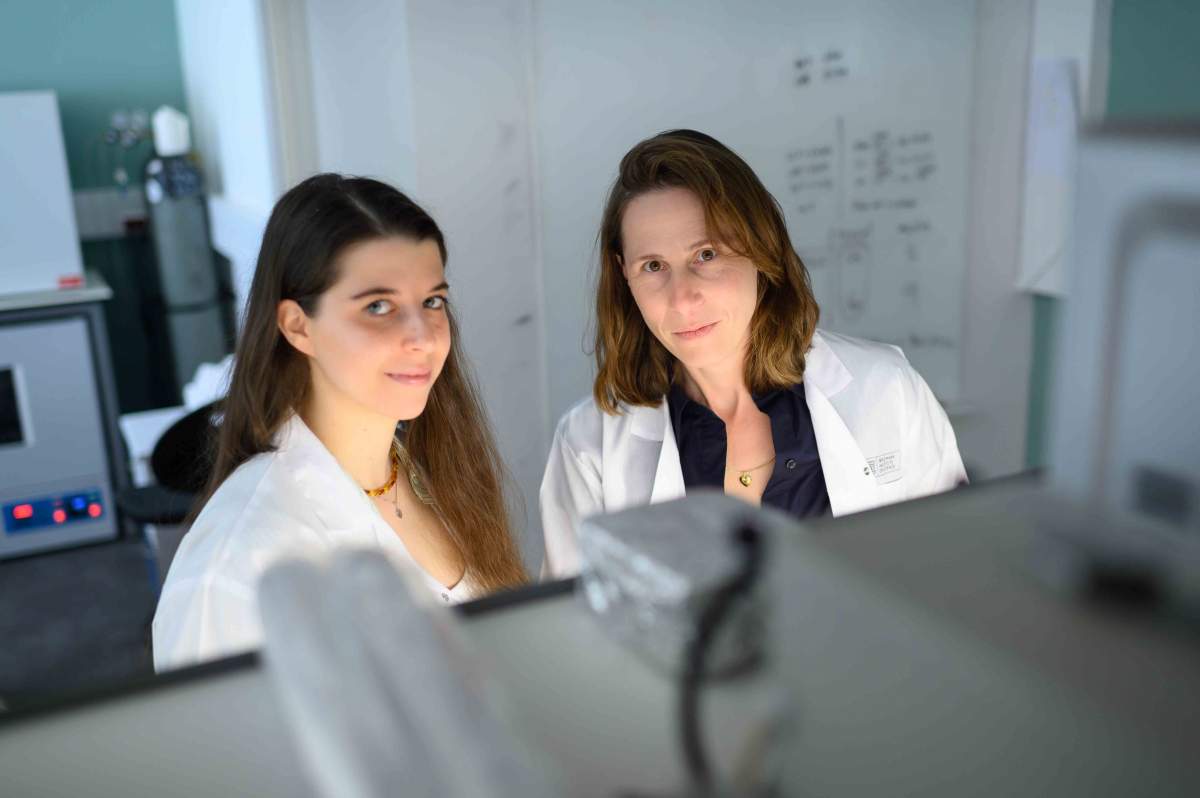
Kedmi hypothesized that the answer must be sought in a type of cell she had discovered during her postdoctoral studies: ROR-gamma-t cells, whose exact lineage is still unknown. This hunch proved true. In their new Nature study, Kedmi’s team in Weizmann’s Systems Immunology Department, led by master’s student Anna Rudnitsky, showed that ROR-gamma-t, rather than conventional dendritic cells, set off the tolerance mechanism. When Rudnitsky eliminated the ability of these particular cells to present food particles to the immune system in mice, the animals rapidly developed food allergies.
“Apparently, there is much more division of labor in the immune system than previously appreciated,” Kedmi explains. “It’s not that dendritic cells always decide whether or not to attack foreign substances. Rather, completely different players – specific, rare cells – are dedicated to launching a mechanism that makes sure we can consume food safely.”
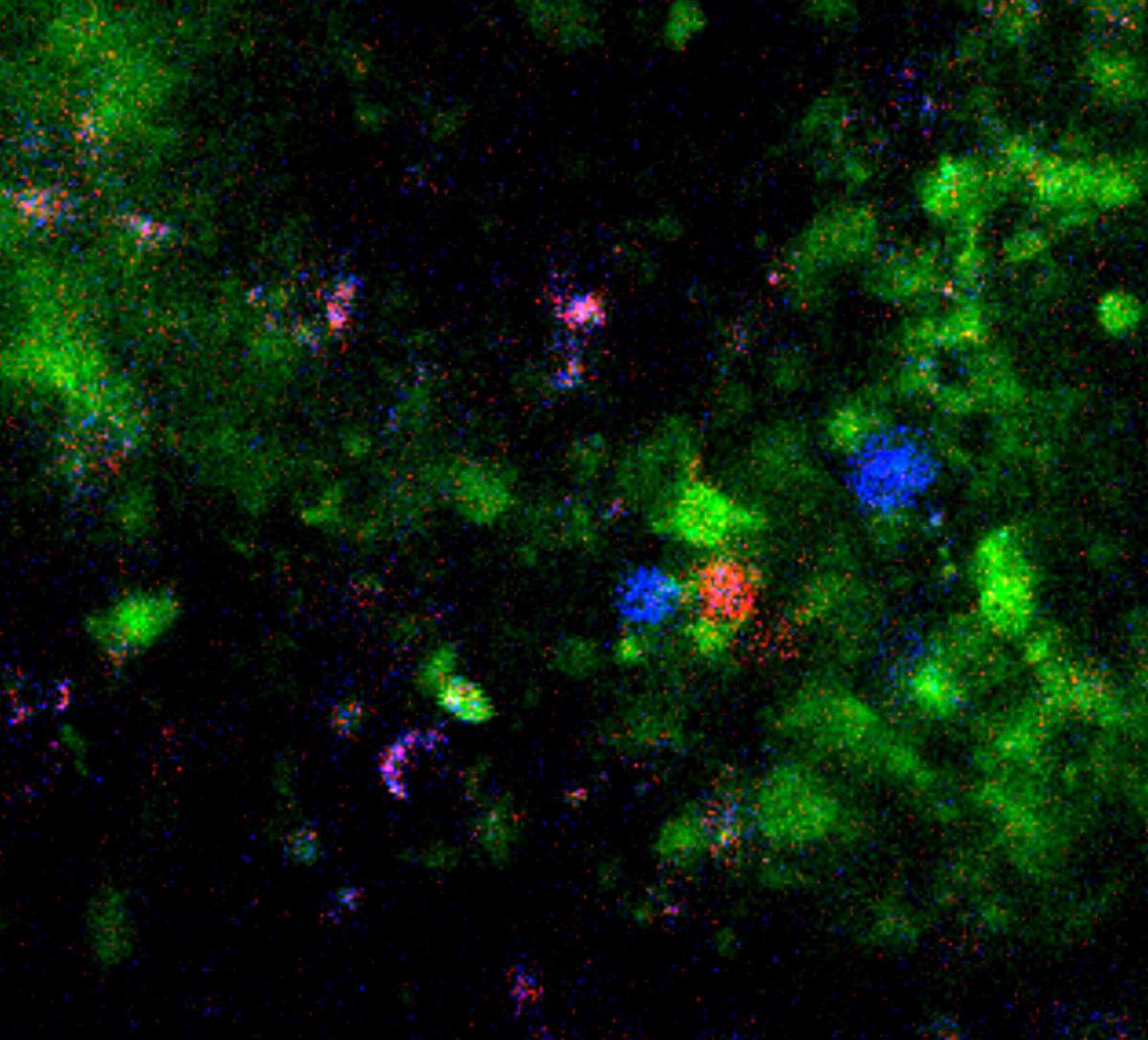
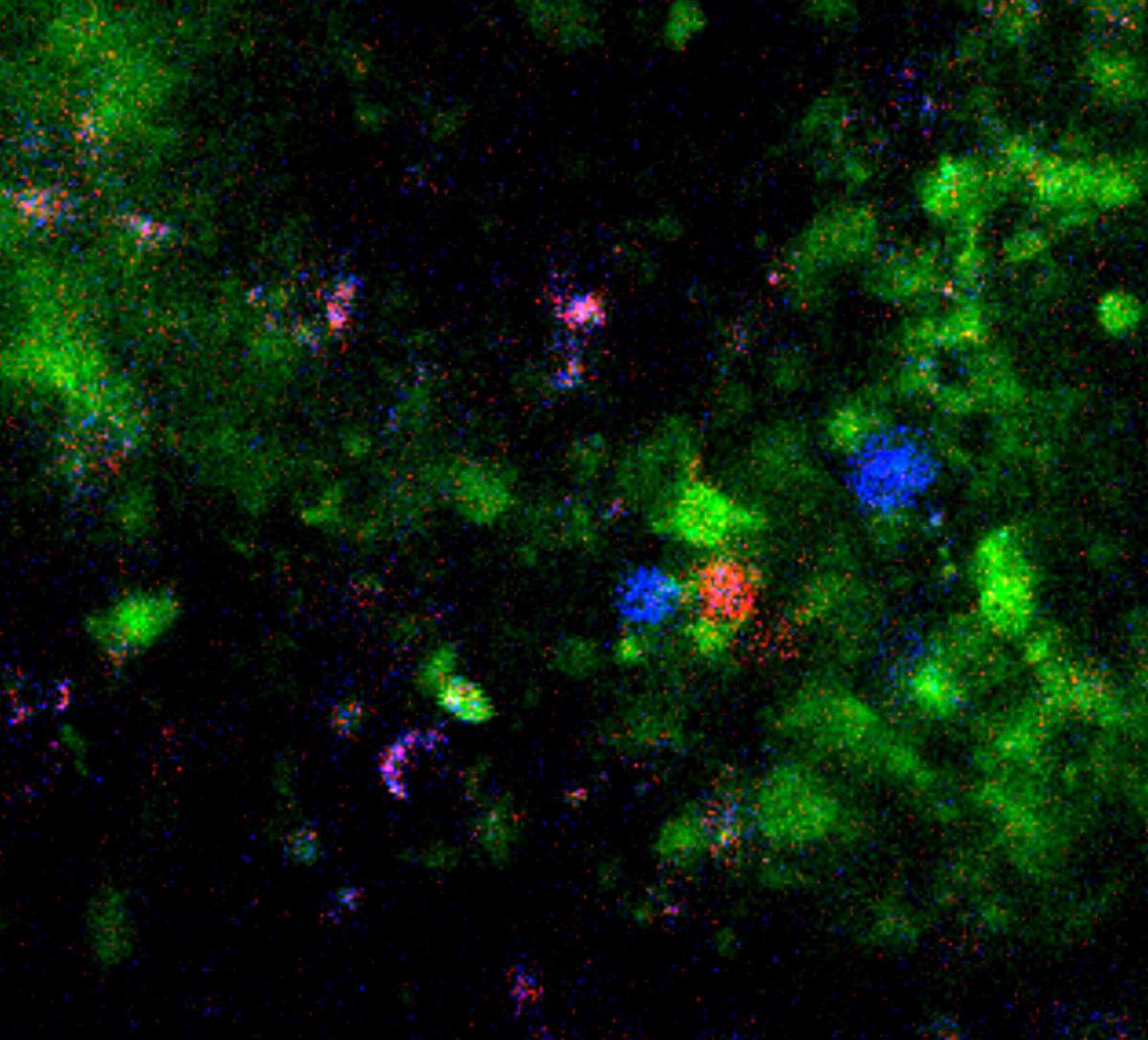
Rudnitsky and the team next aimed to fully decipher the oral tolerance mechanism. By selectively manipulating genes and eliminating different cell types in mice, and then, using advanced genetic tools and microscopy, monitoring cellular responses to food, the researchers identified a coordinated network of four cell types crucial for preventing immune reactions to food. This network is initiated by ROR-gamma-t cells, and their signals are relayed through two other cell types to ultimately suppress the fourth: the immune system’s militant CD8 cells, normally tasked with killing infected cells or triggering inflammation against perceived threats.
These discoveries, particularly of the last link in the network, raised further intriguing questions for Kedmi. What would happen if the immune system encountered microbial proteins that are similar to food ingredients? How could it effectively fight microbial infection after suppressing the CD8 response to these ingredients? Moreover, if oral tolerance suppresses this immune response, why haven’t microbes evolved to disguise themselves as food to evade CD8’s killing power?

To address these questions, the researchers tested whether mice could develop immunity to a microbe that expresses a protein already identified by the mouse immune system as food. They revealed a remarkable dynamic: Faced with a threat, the mice’s immune systems temporarily suspended the tolerance program, deploying CD8 cells to combat the infection. Only after the infection cleared, did the cellular network enable the tolerance program to resume.
Kedmi uses the analogy of two peaceful neighboring countries: “If an aggressor suddenly fires across the border, that individual will be swiftly neutralized by the other side’s forces, peace accords notwithstanding. The immune system operates on a similar principle. In the face of infection, it prioritizes fighting the disease-causing microbe, temporarily setting aside tolerance mechanisms.”
In essence, Kedmi’s team has discovered a sophisticated, dynamic cellular network that allows the immune system to prevent inflammatory responses to food while simultaneously staying on guard against infection. This discovery opens promising new avenues for research into malfunctions in the oral tolerance mechanism that lead to allergies and diseases. For example, the new findings might help reveal how the final stage of the tolerance mechanism, the suppression of the CD8 cells, fails in celiac disease, causing the CD8s to mistakenly attack the intestinal lining in response to gluten. A detailed understanding of the specific points of failure within the oral tolerance network in all types of food allergies and sensitivities could pave the way for improved treatments.
Study participants also included Hanna Oh, Maya Margolin, Inbar Shteinberg, Dr. Liat Stoler-Barak and Prof. Ziv Shulman from Weizmann’s Systems Immunology Department; and Dr. Bareket Dassa from Weizmann’s Life Sciences Core Facilities Department.