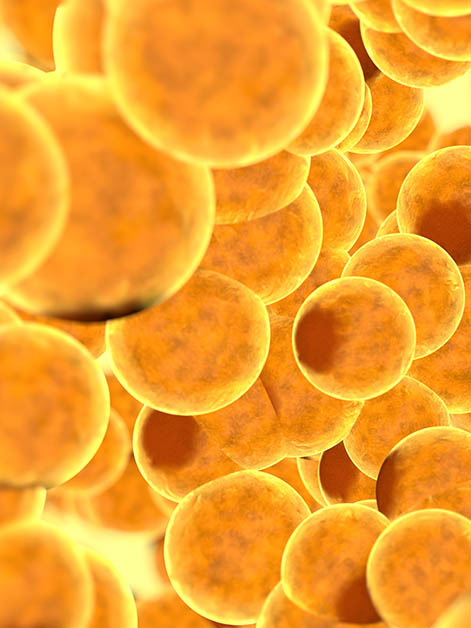
Popular belief holds that our senses gather information only about the external world, but many of our sensory systems also monitor our internal environment, enabling the body to regulate its own functions. In a new study published in Cell Metabolism, researchers from Prof. Elazar Zelzer’s lab at the Weizmann Institute of Science reveal that our nerve cells detect mechanical stimuli, such as pressure and tension, in an unexpected location: the body’s fat tissue. The study also uncovered a surprising link between “fat sense” and obesity: Mice genetically engineered to lack the ability to sense mechanical changes in fat tissue were resistant to obesity and other metabolic conditions, including fatty liver disease.

Not all of the fat in our bodies is “bad.” In fact, there are three major types of fat tissue: White fat serves as the body’s primary energy storage, but it is also associated with obesity and metabolic disorders; brown fat cells, which burn off fats and sugars, keep us warm and ensure that our blood sugar level remains low; and finally, beige fat, which is similar to brown fat, remains dormant within white fat tissue until being activated. Until now, little was known about the connection between the nervous system and the different fat tissues. Scientists understood how the nervous system activates brown fat cells in response to distress, but they didn’t know what commonly suppresses their energy-burning function, causing mice – and humans – to store fat instead of burning it.
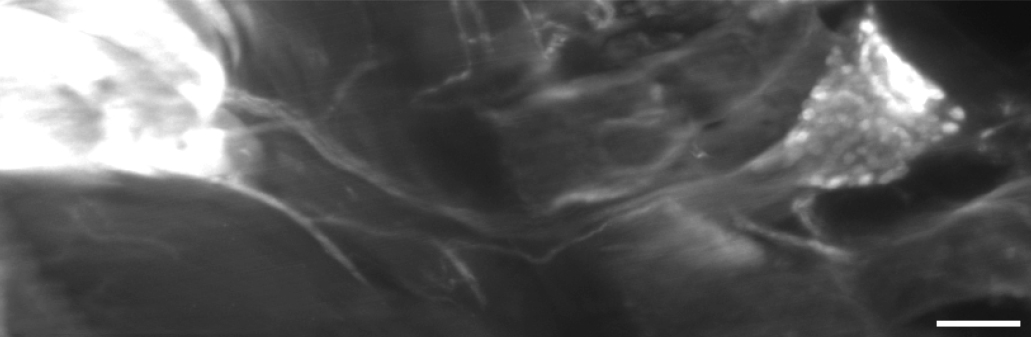
In the new study, the researchers found that sensory nerve cells capable of detecting mechanical forces, such as pressure and tension, send their long extensions into fat tissue. The scientists wanted to learn whether this sensing plays a role in regulating brown fat activity. “We developed a mouse model in which these nerve cells are missing,” says study-leader Dr. Fabian S. Passini, from Zelzer’s lab in Weizmann’s Molecular Genetics Department. “As we were breeding these genetically engineered mice, we noted that they accumulated less fat than the control group, even though they ate the same diet and were less active. We identified a decrease in body fat percentage, lower blood sugar levels and increased insulin sensitivity in these mice; this was the kind of metabolic profile that anybody would love to have. This finding led us to hypothesize that sensory cells play a role in the routine suppression of brown fat activity, and that in their absence, energy burning in the body accelerates.”
""It’s difficult to grasp that just as we sense muscles and bones, we can also sense fat tissue – but that’s precisely what we demonstrated"
The researchers found that to carry out their function, the nerve cells found in fat tissue rely on a well-known sensor called Piezo2, which is capable of monitoring mechanical changes. In the next stage of the study, the scientists selectively silenced this sensor and found that the mice remained skinny, with improved metabolic indicators. Moreover, mice lacking Piezo2 were also found to be “immune” to obesity even after they were fed a high-fat diet.
The team then checked whether removing Piezo2 reduced the risk of metabolic disorders linked to obesity. In mice, as in humans, obesity is often accompanied by fatty liver disease, in which fat accumulating in the liver leads over time to inflammation and scarring. But in mice lacking Piezo2, there was no accumulation of fat drops in the liver and no signs of fatty liver disease, even when they were given a diet high in fat. Despite consuming large quantities of fat for several months, these mice remained sensitive to insulin.
“Until now, we were familiar with the nervous system’s gas pedal, which is responsible for activating brown and beige fat,” explains Zelzer. “But ultimately, we store fat instead of burning all our energy resources, which suggested that there must also be a brake that suppresses metabolism. In our new study, we identified that this brake is actually nerve cells equipped with the Piezo2 sensor, which monitor mechanical changes in brown and beige fat.” The researchers do not know yet which mechanical changes the sensors in fat tissue are detecting, but it is important to recognize that, despite being commonly perceived as passive, fat tissue is actually dynamic and its stiffness can vary depending on the extent of activity in the tissue.
“It’s difficult to grasp that just as we sense muscles and bones, we can also sense fat tissue in our bodies and adjust energy use accordingly – but that’s precisely what we demonstrated in mice,” says Zelzer. “It has long been known that fat affects the body’s energy balance, but previous research primarily focused on hormones secreted by fat tissue, such as leptin. In contrast, neural sensing of fat tissues is much faster and more immediate. More than half (54 percent) of adults in OECD countries are overweight or obese. By understanding the cells that sense fat tissues, we may be able to influence them in ways that will help fight obesity and its related health problems.”