Any virtue taken to an extreme can become a flaw. Take, for instance, stem cells. They hold tremendous promise for repairing or even replacing diseased tissues, by virtue of being flexible and ready to grow. But left unchecked, this same growth can become a hazard: It can lead to cancer.
A new Weizmann Institute study might help avoid this danger. As reported recently in
Cancer Research, the scientists, in collaboration with researchers from the Chaim Sheba Medical Center,
have identified genetic markers that, for a certain type of stem cell, make it possible to predict the risk of any particular cell turning cancerous.
These cells, called mesenchymal stromal stem cells, or MSCs, are particularly attractive for use in therapy. They are almost as versatile as embryonic cells but much more readily available: Found in adults in the bone marrow, skin, fat, muscle and other tissues, they can be removed in large numbers with relative ease. Precisely for these reasons, MSCs are already widely used in clinical trials; for example, they have been transplanted into fetuses to correct a congenital bone disorder. Results have been mixed, partly because the cells fail to survive for a long time after the transplant. But in the future, when scientists learn to improve their survival, a major concern will be to prevent MSCs from causing cancer.
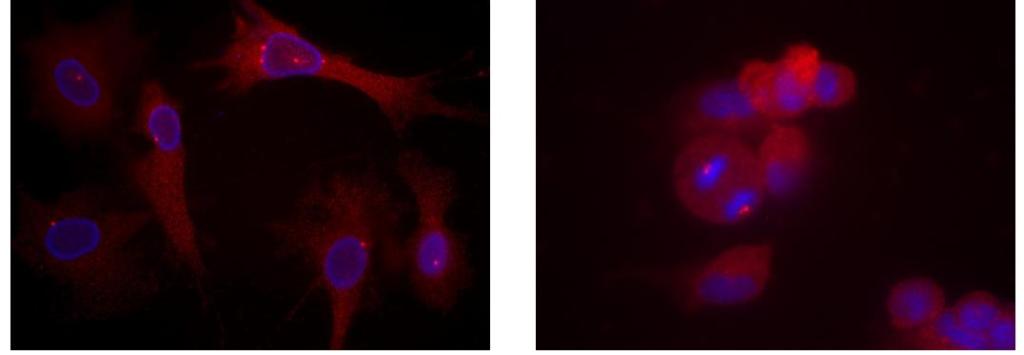
When examining the cancer-causing potential of MSCs in the new study, the scientists were in for a surprise. Overall, cancer-causing MSCs were rare. However, diploid MSCs – that is, those with the normal number of chromosomes – were much more prone to turning cancerous than the polyploid ones – cells that have three or four copies of each chromosome instead of the usual two and that traditionally have been associated with cancer.
The scientists have identified a genetic marker that could be used to distinguish diploid cells from polyploid – a gene called H19: Its activity was more than a thousand times greater in diploid than in polyploid cells. H19 was also found to be a good indicator of a cell’s cancer-causing potential. In fact, when the scientists artificially prompted a diploid cell to become polyploid, its H19 levels dropped – and so did its tendency to turn malignant. H19 measurements can therefore serve as a means of selecting “safe” MSCs, ones with the lowest risk of causing cancer.
The idea that an abnormal number of chromosomes actually leads to less cancer goes against prevalent scientific thinking: How is it possible that the study’s findings run so counter to existing views on polyploidy and cancer?
“Polyploidy is not a direct cause of cancer – on the contrary, it’s probably one of the many strategies used by cells to avoid cancer under stress,” says lead study author
Prof. Dov Zipori of the Molecular Cell Biology Department, a pioneer of adult stem cell research. He and his colleagues propose the following explanation: When exposed to environmental stress, such as UV radiation or exposure to chemical carcinogens that can cause mutations in its DNA, the cell responds by duplicating its chromosomes. If the duplication occurs before the mutation, polyploidy has a protective effect: The cell now has much more DNA than before, so that the effect of the mutation is “diluted” by the newly created mass of genetic material. If, on the other hand, the duplication takes place after the mutation has been introduced, the protective strategy fails: The mutation is multiplied together with polyploidy and can lead to cancer.
In any event, what emerges from the study is that polyploidy in itself is not a predictor of cancer. Rather, the opposite is true: It is a sign that a cell has confronted stress and in some cases, though not all, successfully avoided malignancy.
The study was performed in mice in Zipori’s laboratory by Dr. Ofer Shoshani with the Weizmann Institute’s Hassan Massalha, Dr. Nir Shani, Sivan Kagan, Drs. Orly Ravid, Shalom Madar and Dena Leshkowitz, together with Prof. Gideon Rechavi and Dr. Luba Trakhtenbrot of the Sheba Medical Center.
If confirmed in further studies, this research could increase the safety of stem cell use in a variety of therapies, as well as giving scientists a better understanding of the cellular events that might lead to cancer.
Prof. Dov Zipori's research is supprted by the Helen and Martin Kimmel Institute for Stem Cell Research, which he heads; the Leona M. and Harry B. Helmsley Charitable Trust; David and Molly Bloom, Canada; and Roberto and Renata Ruhman, Brazil. Prof. Zipori is the incumbent of the Joe and Celia Weinstein Professorial Chair.