עיתונאיות ועיתונאים, הירשמו כאן להודעות לעיתונות שלנו
הירשמו לניוזלטר החודשי שלנו:
They volunteer in the largest army in the world. They don't get uniforms, or boots, or a paycheck, but they're heavily armed. They patrol, check identification, isolate and render harmless all suspicious objects, and fight every battle to the death. Their mission: to guard against invasion. Their unit name: the immune system.
As in any army, however, mistakes are made. Communication breaks down and casualties result from friendly fire. Physicians generally lack information about the immune system’s overall battle plan, relying instead on limited information obtained through the questioning of a few scouts. “Medical strategies could be more effective with global information about the system,” says Prof. Irun Cohen of the Immunology Department. Meanwhile, researchers at the Weizmann Institute have developed a way to eavesdrop on the immune system's communication network for clues about the battles being waged.
Communications are critical, for instance, to antibodies, the specialized soldiers of the immune system. Antibodies fight against foreign agents (antigens), but they must be trained to distinguish antigens from normal parts of the body (self-antigens). One small breakdown in identification or communication can trigger an autoimmune response – a deadly attack on self-antigens. Autoimmune diseases are typically chronic and range from slight allergies, to painful and disfiguring diseases like rheumatoid arthritis and multiple sclerosis, to potentially fatal diseases like diabetes. One’s susceptibility or resistance is dependent on the collective state of the immune system, which may be vulnerable for a number of reasons, ranging from inheritance to lifestyle.
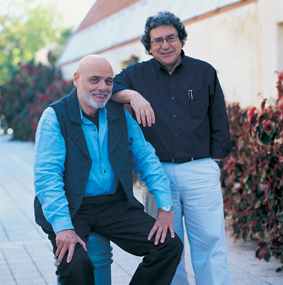
Recognizing that an effective defense initiative requires cooperation, Cohen formed an alliance with Prof. Eytan Domany of the Physics of Complex Systems Department. Drawing upon their combined knowledge of biology, immunology, bioinformatics and physics, the two researchers teamed up to develop a comprehensive analysis of the immune system. They hoped to find patterns in an individual’s repertoire of antibodies that might make it possible to predict resistance or susceptibility to various diseases.
The team elected to study Type 1 diabetes. Prediction is particularly important for diabetes because most of the pancreatic cells producing insulin have already been destroyed by the disease by the time the patient experiences any symptoms. There is no cure, and the prognosis is lifelong insulin dependence, susceptibility to kidney damage, loss of eyesight, leg amputation, coma and death.
In their first collaborative study, the two groups obtained the “immune fingerprints” of both diabetic and healthy subjects – finding each person’s unique complement of antibodies by testing blood samples for interaction with 80 different antigens. They were able to demonstrate that such fingerprints can be used to identify diabetic subjects. This type of trial, however, is very labor-intensive, making it impractical for large-scale, multiple-antigen testing.
Cohen’s lab, therefore, took the lead in developing a chip that would allow testing for a large number of antibodies. The antigen chip contains many hundreds of minuscule antigen dots. Each of these dots attracts a different antibody out of a blood sample, which will hook on to it, just as it would attach to a natural antigen in the body. Researchers from Domany's lab assisted in perfecting the chip for clear and consistent results – a process that took eight months to complete. In theory, data from this exercise could be used to create an extensive profile of an individual’s immune system and perhaps even enable a physician to predict susceptibility to various diseases before they develop.
Obtaining a reading entails shining a laser light on the chip, which gives researchers information not only about the presence of antibodies that bind to the antigens printed on each spot, but also about their relative concentrations. The chip yields unwieldy quantities of information, so to make sense of the numbers, Domany’s group used an algorithm they developed to detect clusters and patterns in large amounts of data. From the original hundreds of antigens, 27 could be used to predict into which of two groups tested mice would fall: those that would become diabetic in the future and those endowed with resistance to the disease.
The researchers credit their in-vention to the cross-fertilization of ideas between their respective scientific fields: “Our multi-disciplinary approach,” says Domany, “led to new questions and new methods for finding answers.”
“Solutions for many types of illnesses and diseases have their foundations in understanding the collective behavior of the immune system,” explains Cohen. Armed with antigen chips, immunologists may gain a new advantage in the fight against silent and deadly enemies. The possible applications range from treating autoimmune diseases to fighting bioterrorism.
A number of people were involved over several years in researching and developing the antigen chip; they include Francisco Quintana, Gaddy Getz, Gad Elizur, Ilan Tzafrir, Dafna Tzafrir and Peter Hagedorn.
Prof. Irun Cohen’s research is supported by the Minna James Heineman Stiftung; the Robert Koch Minerva Center for Research in Autoimmune Disease; and Mr. and Mrs. Samuel Theodore Cohen, Chicago, IL. Prof. Cohen holds the Helen and Morris Mauerberger Professorial Chair in Immunology.
Prof. Eytan Domany’s research is supported by the M.D. Moross Institute for Cancer Research; the Yad Abraham Research Center for Cancer Diagnostics and Therapy; and the Ridgefield Foundation, New York, NY. Prof. Domany is the incumbent of the Henry J. Leir Professorial Chair.